Keratoconus Treatments
Keratoconus is a corneal disease that usually affects both eyes and is often asymmetric, non-inflammatory, characterized by corneal tissue degeneration, steepening, thinning of the corneal apex, and protrusion. Due to its non-inflammatory nature, there is no inflammation or vascularization in the cornea. Keratoconus is derived from the Greek words cornea (kerato) and apex (conus). This structural defect of the cornea results in irregular astigmatism and myopia, which impair vision quality. The onset of keratoconus is gradual, and symptoms usually appear in young adulthood, typically between the ages of 15 and 17. Although it mostly follows a bilateral but asymmetric course (one eye is more affected), it can also be found in one eye in initial cases.
The disease typically progresses for years and then stabilizes. Keratoconus usually plateaus in the 30s or 40s, but it can start, progress, or plateau at any age. Initially, vision can be corrected with glasses or soft lenses, but most patients require rigid, gas-permeable contact lenses to achieve adequate vision. In approximately 20% of these patients, progression continues, and a corneal transplant is required.
Incidence
The gradual onset of keratoconus and the fact that mild cases are often undiagnosed make it difficult to estimate the true frequency. Although the frequency of keratoconus varies by region, the most reliable data is available in the United States, and the estimated frequency is 54.5 per 100,000 people. That is, 54.5 out of 100,000 healthy populations develop keratoconus. Studies show this rate varies up to 230 per 100,000. One study reported that keratoconus is more common in men. It has also been shown that the most frequent age of onset in men is between 15 and 24, and in women between 25 and 34. However, keratoconus is more common in the geographical area including the Middle East and Turkey. Allergic eye diseases that may accompany keratoconus are also more common in this geographical region.
Risk Factors
Genetics and microtraumas are held responsible (Tables 1 and 2). It has also been reported that these patients have an excess of enzymes responsible for inflammation and tissue destruction within the cornea, or that the protective enzymes that prevent the effect of these enzymes are few or non-existent. It has been shown that such destructive radicals increase with sunlight or eye rubbing. Eye rubbing is known to be common in keratoconus patients. Keratoconus is more common in atopic patients (a concept related to diseases such as hay fever, asthma, urticaria, and eczema). Chronic eye rubbing has been linked to keratoconus and may cause the disease to flare up. Frequent eye rubbing, especially in childhood, should be noticed by parents and examined by an ophthalmologist for allergic eye disease-hay fever. Timely precautions prevent the development of keratoconus or prevent its aggravation. Association with some systemic diseases has been reported.
A positive family history is reported as 6%-23%. In fact, the fact that mild keratoconus cases are mostly not detected among family members underestimates the true inheritance frequency. For this reason, if keratoconus is detected, other family members should also be screened for keratoconus.
Table 1. Risk factors
| Contact lenses |
| Eye rubbing |
| Atopy |
| Leber congenital amaurosis |
| Mitral Valve Prolapse |
| Positive Family History |
Table 2.
| Normal | Keratoconus | |
| Eye Rubbing | %58 | %80 |
| Positive Family History | %0.05 | %10 |
Symptoms
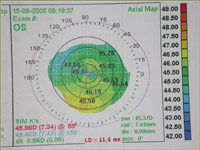
Symptoms vary greatly and depend on the severity of the disease. In the early stages, there are often no findings. During these periods, the diagnosis is made either incidentally while taking a corneal map (Topography) or while investigating the reasons such as changes in eye numbers, the emergence of the patient's incompatible eye numbers, decreased vision, headache, and inability to see clearly with correction. In advanced cases, significant distortion in vision and deep vision loss develop.
However, complete blindness never develops. Generally, no symptoms are encountered in mild keratoconus cases. In moderate and advanced keratoconus cases, the ophthalmologist may encounter the following corneal findings.
Cone-shaped protrusion
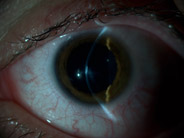
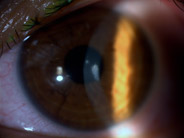
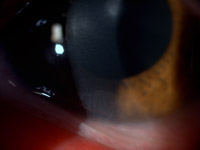
In advanced keratoconus, this appearance is easily noticed with a biomicroscope or with the naked eye when the patient looks down (Munson's sign).
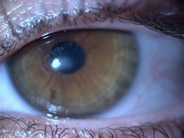
Thinning
Iron deposits
Vogt's striae (Vertical lines in the deep cornea)
Scarring (Apical scar)
 |
 |
 |
|
Distorted vision in keratoconus eye. |
Munson's sign |
Thinning and protrusion in the cornea (Pentacam image) |
|
|
|
|
|
|
|
|
|
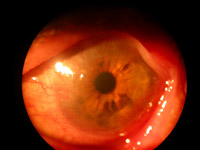
Scar in the center of the cornea |
||
Sometimes, excessive steepening and thinning cause cracking in the deep layers of the cornea and the entry of intraocular fluid into the cornea, resulting in swollen and blurred cornea formation due to edema (Hydrops see Figure). Edema can last for weeks or months and disappears leaving a scar. Corneal hydrops does not constitute an indication for keratoplasty; even the resulting scar can flatten the cornea and facilitate contact lens use.
|
|
|
|
|
Hydrops |
||
 |
|
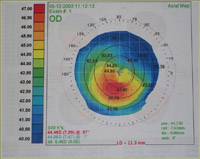
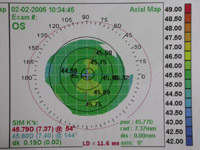
Topographic appearance in a keratoconus case |
Diagnosis
Even in the earliest stages, the diagnosis is easily made with topography (corneal mapping).
Differential Diagnosis
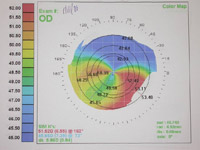
Keratoconus should be differentiated from other ectatic diseases of the cornea that manifest with thinning. Unlike the others, in keratoconus, corneal thinning and steepening are central. These are pellucid marginal degeneration, Terrien's marginal degeneration, and keratoglobus. Sometimes, irregularities that may occur in the cornea due to lens use after contact lens use (Contact lens warpage) can be mistaken for keratoconus.
|
|
 |
 |
||
|
Pellucid marginal degeneration |
Terrien's marginal degeneration |
|||
|
|
 |
||
|
The irregularity in the topography is seen to improve after stopping CL |
|||
Treatment
Treatment varies depending on the severity of the disease. First, underlying eye disorders such as allergic conjunctivitis and dry eye, which may cause microtraumas and eye rubbing, should be treated. Patients should be prevented from rubbing their eyes. Allergic eyes also reduce lens tolerance.
Rigid contact lenses are the main step in treatment. Although glasses are sufficient to correct visual impairment in very early stages, rigid lenses are needed to correct irregular astigmatism that occurs with the progression of the disease. Usually, the vast majority of patients benefit from rigid lenses. However, contact lens fitting is complex in keratoconus. Patients can usually get used to rigid lenses over time.
Serious complications related to rigid lenses are rare. Problems encountered include corneal abrasion (abrasion), apical scar (scar in the center of the cornea), vascularization, lens-related discomfort, and the lens not staying on the cornea for a sufficient period. Correct adjustment of contact lenses is important, otherwise, there is destruction in the cornea and progression in keratoconus.
|
|
 |
|
|
The irregularity in the topography is seen to improve after stopping CL |
Limbal insufficiency due to long-term lens use |

 Türkçe (TR)
Türkçe (TR)